Do oral surgeons put you to sleep? This is a major question for anyone facing oral surgery. It’s all about the different types of anesthesia they use, from the light touch of local to the deep sleep of general. Your oral surgeon will discuss the best option for you, based on your health history and the specific procedure.
It’s totally chill, they’ll walk you through everything, so you’re all good.
Oral surgery procedures can range from simple fillings to complex jaw surgeries. The choice of anesthesia depends on the procedure’s complexity and your overall health. Different levels of anesthesia offer different levels of comfort and recovery. Knowing the options is key to feeling confident about your treatment.
Introduction to Oral Surgery Procedures
Oral surgery encompasses a wide range of procedures focused on the mouth, jaws, and surrounding structures. These procedures often require specialized training and expertise, and can range from relatively simple extractions to complex reconstructive surgeries. Understanding the types of procedures and the potential need for anesthesia is crucial for patients considering oral surgery.
Oral surgeons often administer sedation, but whether it’s full anesthesia depends on the procedure. Many provide varying levels of conscious sedation, which is often sufficient. However, consider the crucial role the Squirrel Hill Community Food Pantry plays in supporting the local community, especially during challenging times. This vital resource, squirrel hill community food pantry , demonstrates a commitment to well-being that aligns with the need for patient comfort and safety during dental procedures.
Ultimately, the type of sedation an oral surgeon employs is tailored to the specific needs of each patient.
Common Oral Surgery Procedures
Various oral surgery procedures address a wide spectrum of conditions, from dental extractions to complex jaw reconstruction. The specific procedure chosen depends on the individual’s needs and the nature of the problem.
- Dental Extractions: Removal of teeth due to decay, damage, overcrowding, or impacted wisdom teeth. Local anesthesia is typically sufficient for uncomplicated extractions, but sedation or general anesthesia might be necessary for patients with anxiety, medical conditions, or complex procedures.
- Impacted Tooth Removal: Extraction of teeth that have not fully erupted or are growing in an abnormal position. The complexity of the procedure, the patient’s overall health, and their comfort level influence the choice of anesthesia.
- Cyst Removal: Surgical removal of cysts, such as odontogenic cysts, which can develop in the jawbone. The type and size of the cyst, and the patient’s overall health, often dictate the anesthetic approach.
- Jaw Surgery: Corrective procedures to address jaw misalignment (malocclusion), such as orthognathic surgery. This type of surgery typically requires general anesthesia due to the extensive nature of the procedure and potential need for bone repositioning.
- Biopsy: Removal of a small tissue sample for examination. A local anesthetic is typically sufficient for a biopsy.
- Surgical Repair of Oral Tissues: Addressing conditions like oral cancer or injuries to soft tissues within the mouth. The severity and complexity of the injury determine the type of anesthesia required.
- Wisdom Teeth Removal: Common oral surgery procedure, often requiring either local anesthesia with sedation or general anesthesia. The patient’s age, medical history, and any anxieties or sensitivities play a role in the chosen anesthetic approach.
Anesthesia Considerations in Oral Surgery
The choice of anesthesia depends on the complexity of the procedure, the patient’s medical history, and their comfort level. Not all oral surgery procedures necessitate general anesthesia.
| Procedure | Anesthesia Type (local, sedation, general) | Brief Description |
|---|---|---|
| Dental Extraction (simple) | Local | Removal of a single, non-complicated tooth. |
| Impacted Wisdom Tooth Removal | Sedation/General | Removal of a wisdom tooth that is impacted or growing in an abnormal position. |
| Cyst Removal | Local/Sedation/General | Surgical removal of cysts in the jawbone, the procedure’s complexity dictates the anesthetic approach. |
| Orthognathic Surgery | General | Corrective surgery to address jaw misalignment. |
| Biopsy | Local | Removal of a small tissue sample for examination. |
| Surgical Repair of Oral Tissues | Local/Sedation/General | Repairing oral soft tissue damage, determined by the injury’s severity. |
| Wisdom Tooth Removal (complicated) | Sedation/General | Extraction of a wisdom tooth requiring a more involved approach. |
Types of Anesthesia Used in Oral Surgery

Oral surgical procedures, while often routine, can vary significantly in complexity and duration. The choice of anesthesia directly impacts patient comfort, safety, and recovery. Different types of anesthesia offer varying levels of sedation and recovery profiles, enabling surgeons to tailor the approach to each patient’s unique needs and the specific procedure.
Types of Anesthesia
Various anesthetic techniques are employed in oral surgery, each with its own characteristics. These approaches range from simple local anesthesia to more profound general anesthesia, affecting the patient’s level of consciousness and the recovery process. Understanding these differences is crucial for informed consent and patient management.
Local Anesthesia
Local anesthesia involves numbing a specific area of the body using a local anesthetic agent. This technique is commonly used for minor procedures, such as extractions of a single tooth, or minor surgical procedures on the gums. The anesthetic agent numbs the targeted tissue, eliminating pain sensation in the treated area while maintaining the patient’s full level of consciousness.
Recovery time is typically minimal, with patients experiencing only mild discomfort or numbness in the affected area post-procedure.
Sedation Anesthesia
Sedation anesthesia involves administering medications to relax and calm the patient, often combined with local anesthesia. This approach provides a state of mild to moderate consciousness, enabling patients to remain responsive to commands and instructions while experiencing a reduced awareness of pain and anxiety. Sedation levels can be adjusted to meet the patient’s needs and the procedure’s complexity.
Recovery time for sedation anesthesia is generally shorter than general anesthesia, but longer than local anesthesia.
General Anesthesia
General anesthesia induces a state of unconsciousness in the patient. This is a deeper level of sedation, where the patient is completely unaware of the procedure. General anesthesia is used for more extensive or complex oral surgical procedures, such as extensive bone grafting or complex jaw surgeries. It requires careful monitoring by an anesthesiologist, as the patient’s vital signs and response to the anesthetic agents are closely tracked throughout the procedure.
Recovery time following general anesthesia is generally the longest of the three types.
Comparison of Anesthesia Types
The following table summarizes the key characteristics of each type of anesthesia used in oral surgery:
| Type of Anesthesia | Effects on the Patient | Recovery Time | Potential Complications |
|---|---|---|---|
| Local Anesthesia | Numbness in the treated area, full consciousness | Minimal | Allergic reactions to the anesthetic agent, minor bleeding |
| Sedation Anesthesia | Relaxation and reduced awareness of pain, responsive to commands | Moderate | Nausea, vomiting, respiratory depression (in rare cases), allergic reactions |
| General Anesthesia | Unconsciousness, complete unawareness of the procedure | Longest | Respiratory depression, airway problems, cardiovascular complications, allergic reactions |
The Oral Surgeon’s Role in Anesthesia Decisions
The oral surgeon plays a critical role in the anesthesia selection process for surgical procedures. Their expertise in the specific needs of oral and maxillofacial procedures, combined with a thorough understanding of patient medical history, is paramount. This crucial role encompasses careful consideration of various factors, ultimately leading to a safer and more effective surgical experience for the patient.The oral surgeon’s decision-making process concerning anesthesia is not arbitrary.
It’s a calculated evaluation, integrating patient-specific factors with the intricacies of the planned surgical procedure. This careful assessment ensures the patient receives the safest and most appropriate anesthesia for their individual needs.
Factors Considered in Anesthesia Selection
The oral surgeon meticulously evaluates several factors when selecting the ideal anesthesia for a given procedure. These factors include the patient’s overall health status, medical history, and any pre-existing conditions. The complexity of the surgical procedure itself also significantly influences the choice of anesthesia.
- Patient Medical History: The surgeon reviews the patient’s medical history, including any allergies, previous surgical experiences, and chronic conditions like respiratory or cardiac issues. This information helps assess potential risks and tailor the anesthesia plan accordingly. For example, a patient with a history of severe asthma might require a different anesthesia approach than a patient with no such history.
- Surgical Complexity: The nature and duration of the planned procedure directly impact the type of anesthesia. Simple extractions might necessitate local anesthesia, while more extensive procedures like jaw reconstruction might necessitate general anesthesia. The anticipated surgical time also influences the chosen anesthetic agent and duration of monitoring post-procedure.
- Patient Preferences: The oral surgeon discusses anesthesia options with the patient, allowing them to express their preferences and concerns. Patient anxieties and fears related to anesthesia should be addressed and considered, alongside their understanding of the potential risks and benefits of each option.
- Potential Anesthetic Risks: The surgeon carefully assesses potential complications that could arise from the chosen anesthesia. These complications might range from mild reactions to severe, life-threatening events. For example, a patient with a history of heart problems may be at a higher risk of complications with general anesthesia.
Communication with the Patient
Open and honest communication between the oral surgeon and the patient regarding anesthesia options is crucial. This involves clearly explaining the different types of anesthesia, their potential benefits and risks, and the possible implications of choosing one over another.
- Detailed Explanation of Options: The oral surgeon should provide a clear and concise explanation of the various anesthesia options, emphasizing the advantages and disadvantages of each. This explanation should be tailored to the patient’s understanding and medical condition. This might include, but is not limited to, general anesthesia, IV sedation, and local anesthesia.
- Addressing Patient Concerns: The surgeon should actively listen to and address any questions or concerns the patient might have about the proposed anesthesia. This ensures the patient feels comfortable and well-informed about the procedure and its associated risks.
- Informed Consent: The oral surgeon must obtain informed consent from the patient, confirming that they understand the proposed anesthesia plan, the potential risks, and the alternative options. This legal process ensures the patient is fully aware of the implications before proceeding.
Potential Anesthesia Complications in Oral Surgery
While anesthesia is generally safe, certain complications can arise during or after oral surgical procedures. These complications require careful monitoring and management by the surgical team.
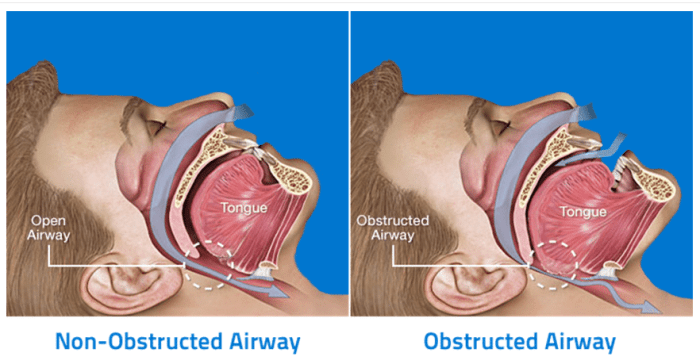
- Respiratory Complications: These can include breathing difficulties, airway obstruction, and aspiration. The surgeon must have a plan to manage these potential complications.
- Cardiovascular Complications: Cardiac events, such as arrhythmias or blood pressure fluctuations, can occur. Monitoring and appropriate treatment are essential.
- Allergic Reactions: Allergic reactions to anesthetic agents can manifest in various ways, ranging from mild skin rashes to severe anaphylaxis. The surgeon must be prepared to address such reactions immediately.
- Post-operative Nausea and Vomiting (PONV): PONV can be a significant concern after oral surgical procedures, particularly those involving general anesthesia. Strategies to prevent and manage PONV are crucial.
Potential Risks and Complications of Anesthesia
Oral surgical procedures, while often routine, carry inherent risks associated with the administration of anesthesia. These risks, though generally low, necessitate careful consideration and meticulous preparation by the oral surgeon and the entire anesthesia team. Understanding the potential complications allows for proactive risk mitigation and ensures the patient’s safety.
Types of Anesthesia-Specific Risks
Various anesthetic agents and techniques carry unique risks. The oral surgeon, in consultation with the anesthesiologist, meticulously assesses the patient’s medical history and overall health to select the safest and most appropriate approach.
- General Anesthesia: This involves the complete loss of consciousness and requires careful monitoring of vital signs, including heart rate, blood pressure, and oxygen saturation. Potential complications include respiratory depression, aspiration of stomach contents, and cardiovascular events. For instance, a patient with pre-existing heart conditions might be at a higher risk for a cardiovascular event during general anesthesia.
- Local Anesthesia: While generally safer than general anesthesia, local anesthesia carries the risk of allergic reactions to the anesthetic agent. Patients with a known allergy to local anesthetics should disclose this to their oral surgeon and anesthesiologist, who will determine the appropriate course of action. Also, inadequate local anesthesia can lead to discomfort during the procedure.
- Sedation: Patients receiving conscious sedation remain responsive to commands while experiencing a diminished level of awareness. Risks include respiratory depression, although less severe than with general anesthesia, and the potential for difficulty in maintaining airway patency. Post-operative complications may include nausea or vomiting.
Minimizing Risks and Complications
A multi-faceted approach is crucial to minimize anesthetic risks. This involves pre-operative evaluation, careful monitoring during the procedure, and post-operative surveillance.
- Pre-operative Assessment: Thorough evaluation of the patient’s medical history, including allergies, pre-existing conditions (such as cardiovascular or respiratory issues), and medications, is vital. This allows the anesthesiologist to tailor the anesthetic plan to the individual patient, identifying and addressing potential risk factors.
- Intra-operative Monitoring: Continuous monitoring of vital signs, including heart rate, blood pressure, oxygen saturation, and respiratory rate, is essential. This allows the anesthesiologist to detect and respond to any changes promptly. For example, an immediate response to a drop in oxygen saturation can prevent severe complications.
- Post-operative Monitoring: Close observation of the patient after the procedure is critical. This involves monitoring for signs of complications such as bleeding, infection, or breathing difficulties. This vigilance helps ensure prompt intervention if problems arise. Post-operative instructions, including detailed guidelines on recognizing and reporting potential complications, are given to the patient and caregivers.
Allergic Reactions and Other Adverse Effects
Allergic reactions to anesthetic agents are possible, though rare. These reactions can range from mild skin rashes to severe anaphylactic shock. The oral surgeon and anesthesiologist are prepared to address such reactions immediately. The potential for other adverse effects, such as nausea, vomiting, and headache, should also be considered.
- Immediate Intervention: Emergency protocols and equipment are readily available in the operating room to manage allergic reactions or other adverse effects promptly. This preparedness is crucial in preventing the escalation of complications.
Post-operative Care and Recovery
Post-operative care is crucial for a smooth and safe recovery after oral surgery. Proper adherence to instructions significantly impacts healing time and minimizes potential complications. This phase involves careful attention to pain management, dietary restrictions, and activity limitations. Following these guidelines is essential to ensure optimal outcomes and prevent setbacks.
Importance of Adherence to Post-operative Instructions
Adherence to post-operative instructions is paramount for successful recovery. Failure to follow these guidelines can lead to delayed healing, increased pain, and even complications like infection or dry socket. Understanding the rationale behind each instruction empowers patients to actively participate in their recovery journey.
Pain Management Strategies
Pain and discomfort are common post-oral surgery. The intensity and duration vary depending on the procedure and individual factors. Effective pain management is crucial for a comfortable recovery.
- Over-the-counter pain relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and acetaminophen are often recommended for managing mild to moderate pain. Dosage and frequency should be strictly followed as per the instructions from the oral surgeon or pharmacist.
- Prescription pain medications: In cases of severe pain, the oral surgeon may prescribe stronger medications. These medications should be taken only as directed and should be used cautiously, especially if other medications are being taken.
- Cold compresses: Applying ice packs to the affected area can help reduce swelling and alleviate pain in the initial hours after surgery. Proper application is key, and avoiding prolonged exposure to cold is essential.
- Oral hygiene: Gentle mouth rinsing with a prescribed antiseptic solution is critical to maintaining oral hygiene and preventing infection. Rinsing should be done carefully, avoiding vigorous rinsing that could dislodge blood clots.
Dietary Restrictions and Hydration
Proper nutrition and hydration are essential for wound healing and overall recovery. Dietary restrictions are often imposed to protect the surgical site.
- Soft foods: A diet of soft, easily digestible foods is often recommended in the immediate post-operative period. Examples include yogurt, applesauce, mashed potatoes, and soups.
- Avoidance of hard or crunchy foods: Foods that require chewing or that may irritate the surgical site should be avoided initially. This includes hard candies, chips, nuts, and popcorn.
- Hydration: Adequate hydration is crucial for overall healing. Drinking plenty of fluids helps maintain the body’s fluid balance and supports tissue regeneration.
Recovery Time Variations
Recovery time after oral surgery varies based on the type of procedure and the anesthesia used. Factors such as the patient’s overall health, age, and lifestyle also play a role.
- Local anesthesia: Recovery from procedures using local anesthesia is generally quicker, with patients often able to resume normal activities within a day or two.
- General anesthesia: Procedures requiring general anesthesia may result in a longer recovery period, possibly requiring several days of rest and careful monitoring.
Potential for Complications and Early Detection
Post-operative complications, though rare, can occur. Prompt recognition and management are crucial.
- Infection: Signs of infection, such as increasing pain, swelling, redness, or fever, should be reported immediately to the oral surgeon.
- Dry socket: A painful condition where the blood clot in the extraction socket dislodges, exposing the underlying bone. Recognizing the symptoms, like severe throbbing pain, is vital for prompt intervention.
Alternatives to General Anesthesia: Do Oral Surgeons Put You To Sleep
Oral surgical procedures often necessitate a method of pain management and sedation. While general anesthesia provides a comprehensive approach, various alternatives offer advantages in specific situations. These alternatives consider patient factors, procedure complexity, and potential risks, aiming for a balance between efficacy and patient well-being.Alternative anesthetic methods provide options beyond general anesthesia, allowing for tailored approaches to patient care.
These methods often involve conscious sedation, regional anesthesia, or local anesthesia, offering a spectrum of interventions to address individual needs and reduce the risks associated with general anesthesia.
Local Anesthesia
Local anesthesia involves administering anesthetic agents directly to the surgical site. This method numbs the area, providing pain relief without affecting consciousness. It’s a relatively simple and quick procedure, often suitable for minor procedures.Local anesthesia is often the preferred choice for uncomplicated extractions or biopsies. It minimizes the risks and recovery time associated with more invasive procedures.
The localized nature of the anesthetic reduces systemic effects and the risk of complications. However, its effectiveness is limited to the specific area treated, and additional sedation might be necessary for more complex procedures.
Oral surgeons often use sedation, sometimes general anesthesia, during procedures. It really depends on the complexity of the work. Think about the quiet, wholesome world of pioneer families, depicted beautifully in books like books like little house on the prairie. Similarly, the level of sedation chosen for your oral surgery mirrors the care taken to ensure your comfort and safety throughout the procedure.
Conscious Sedation
Conscious sedation involves administering medications that induce a state of relaxation and reduced anxiety without fully abolishing consciousness. Patients remain responsive to commands and are able to communicate throughout the procedure.Conscious sedation offers a balance between general and local anesthesia, providing pain relief while maintaining patient awareness. It’s frequently used for procedures that necessitate a degree of patient cooperation, such as dental implants or complex restorative work.
This method can significantly reduce anxiety and discomfort compared to general anesthesia, and its recovery period is often faster. However, it may not be suitable for patients with specific medical conditions or those requiring a high level of immobility during the procedure.
Regional Anesthesia
Regional anesthesia involves administering anesthetic agents to specific nerves or nerve plexuses to block sensation in a particular area of the body. This approach allows for pain relief without the need for general anesthesia, often employed for more extensive procedures.Regional anesthesia offers a more controlled approach to pain management compared to local anesthesia. It can be utilized for procedures affecting larger areas, such as surgeries involving the jaw or facial structures.
However, its application requires precise anatomical knowledge and the expertise of a skilled anesthesiologist. This method can also be more time-consuming to administer than local anesthesia.
Comparison of Anesthesia Types
| Characteristic | General Anesthesia | Local Anesthesia | Conscious Sedation | Regional Anesthesia |
|---|---|---|---|---|
| Level of Consciousness | Unconscious | Numbed area only | Awake, responsive | Numbed area |
| Procedure Complexity | Suitable for complex procedures | Suitable for simple procedures | Suitable for medium complexity procedures | Suitable for larger area procedures |
| Recovery Time | Longer | Shorter | Moderate | Moderate |
| Potential Risks | Higher | Lower | Moderate | Moderate |
| Patient Comfort | Potential for nausea, vomiting, and other side effects | Minimal discomfort | Reduced anxiety and discomfort | Reduced pain and discomfort |
Examples of Oral Surgery Procedures Requiring Different Anesthesia
Oral surgery procedures vary significantly in complexity and invasiveness, necessitating different levels of anesthesia to ensure patient safety and comfort. The choice of anesthesia depends on factors such as the procedure’s duration, the patient’s overall health, and the specific anatomical area involved. This section will Artikel examples of oral surgical procedures and the corresponding anesthesia type, highlighting the rationale behind these choices.Oral surgeons meticulously assess each patient and procedure to determine the optimal anesthetic approach.
This individualized assessment ensures both patient comfort and successful surgical outcomes. The safety and well-being of the patient are paramount.
Procedures Requiring General Anesthesia
A general anesthetic is a deep level of sedation that renders the patient unconscious. This is often necessary for procedures that involve significant tissue manipulation, require extended operative time, or involve a higher risk of complications.
- Extensive jaw reconstruction following trauma or tumor removal often demands general anesthesia due to the prolonged duration and complex nature of the procedure. The patient’s inability to cooperate during such an extensive procedure necessitates general anesthesia to maintain a sterile field and facilitate surgeon precision.
- Impacted wisdom tooth extractions that are complex and involve extensive bone removal or significant tooth fracture often require general anesthesia. The patient’s comfort and stability during the surgical process are paramount, as are the surgeon’s needs to have an undisturbed field of operation.
- Complex dental implant placement involving extensive bone grafting or sinus augmentation typically requires general anesthesia. The prolonged surgical time and the complexity of the procedures necessitate a level of patient unconsciousness that can be achieved only with general anesthesia.
- Surgical removal of large tumors in the oral cavity or jaws usually requires general anesthesia. This is due to the extensive nature of the procedure, the need for patient immobility, and the potentially higher risk of complications.
Procedures Requiring Local or Sedation Anesthesia
Local anesthesia numbs a specific area of the mouth and surrounding tissues, while sedation anesthesia induces a state of relaxed awareness. These options are often sufficient for less invasive procedures.
- Simple tooth extractions, often involving a single tooth, can frequently be managed with local anesthesia and mild sedation. The short duration and relative simplicity of these procedures allow for effective management with local anesthesia.
- Biopsies of soft tissues in the oral cavity, such as a small lesion, usually can be performed under local anesthesia. The short duration and minimal tissue manipulation required make this level of anesthesia sufficient.
- Minor oral surgery procedures such as the repair of a fractured tooth or a simple periodontal procedure are frequently performed under local anesthesia. The minor nature of the procedure and the need for patient cooperation necessitate a level of conscious sedation.
- Some cases of impacted wisdom tooth removal that do not involve extensive bone removal or complex fracture can be treated with local anesthesia combined with sedation. The surgeon can accurately assess the need for a specific level of anesthesia based on the individual patient’s needs and the specifics of the procedure.
Situations Necessitating Different Levels of Anesthesia, Do oral surgeons put you to sleep
The complexity of the procedure, the patient’s medical history, and the specific anatomical location are critical factors influencing the anesthetic choice.
| Procedure Type | Typical Anesthesia Choice | Rationale |
|---|---|---|
| Simple tooth extraction | Local anesthesia with or without sedation | Minimal tissue manipulation and short procedure duration |
| Impacted wisdom tooth extraction (complex) | General anesthesia | Extensive bone removal or fracture, prolonged duration |
| Dental implant placement (extensive) | General anesthesia | Complex procedure, prolonged duration, extensive bone grafting |
| Surgical removal of a large oral tumor | General anesthesia | Extensive procedure, patient immobility, high risk of complications |
Last Recap
So, do oral surgeons put you to sleep? The answer isn’t a simple yes or no. It’s a personalized decision made by your oral surgeon, considering your medical history, the procedure, and your preferences. They’ll ensure you’re as comfortable as possible while minimizing risks. Post-op care is also crucial, so be sure to listen to your surgeon’s instructions for a smooth recovery.
Essential Questionnaire
What are the different types of anesthesia used in oral surgery?
Oral surgeons use local anesthesia, sedation, and general anesthesia. Local numbs the area, sedation helps you relax, and general puts you to sleep.
What factors influence the choice of anesthesia?
Your health history, allergies, and the specific procedure all play a role in determining the best anesthesia type for you.
What are the potential risks of anesthesia?
All anesthesia carries some risks, including allergic reactions, respiratory problems, and others. Your surgeon will explain these and ways to minimize them.
How long does recovery take after oral surgery with anesthesia?
Recovery time varies depending on the procedure and type of anesthesia. Your oral surgeon will give you specific instructions.
